Occasional constipation is a common and temporary medical problem for most adults. It is more common as we get older with over one third of adults over the age of 60 reporting at least occasional constipation. Typical symptoms are incomplete elimination of stool, difficulty passing stool and hard stools often accompanied by abdominal bloating, pain and distention. Normal stool frequency varies from individual to individual from 3 times a week to 3 times a day. A sudden slowdown in stool frequency not accompanied by a dietary change usually results in the symptoms associated with constipation.
The three main types of primary constipation are normal transit, slow transit and disorders of defecation. The most common and easiest to treat is normal transit where the stools are hard, smaller and straining is involved to push them out. Slow transit is caused by abnormal innervation of the muscles in the bowel leading to poor movement through the colon. To evaluate slow transit constipation sometimes imaging, testing and a specialist consultation is needed to help confirm and treat the underlying problem. Disorders of defecation occur in older people who have a poor rectal reflex or weak pelvic muscle strength making it hard for them to recognize a full rectum and have the power to completely evacuate stool from the rectal vault. This can lead to frequent soiling and overflow problems.
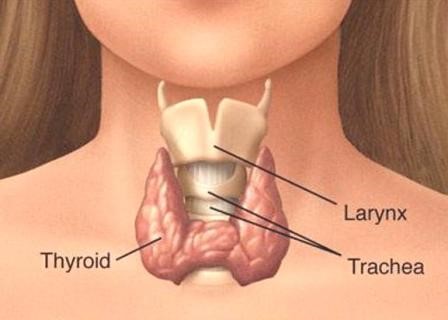
Secondary constipation occurs due to medical conditions like hypothyroidism or diabetes, chronic illnesses or medication side effects. Secondary constipation can usually be ruled out with lab work and routing imaging as well as medication adjustments. Narcotic pain medications most commonly cause constipation as a side effect as do over-the-counter antacids, iron and calcium supplements and some prescription blood pressure medications and muscle relaxers.
Fiber + Fluids + Move = Regularity
Most normal transit constipation can be improved with diet/behavior changes. The three most important items to check off to ensure adequate stool GI motility are:
- Daily exercise activity and avoiding prolonged sitting.
- Getting enough dietary fiber (28 grams for females and 38 grams for males) by eating legumes, nuts, grains, fruits and vegetables.
- Adequate hydration 1.5-2 liters daily.
Other measures include: Warm liquids in the morning, taking advantage of the gastrocolic reflex by scheduling a bathroom trip after meals and while toileting using a stool to lift your feet off the floor to align the anorectal junction to aid passage of stool.
Treatment options:
Need something now
If you are really uncomfortable and need to do something urgently, then I usually recommend a saline, mineral oil or plain water enema with or without 150-300 milliliters of magnesium citrate single dose or split dose of 150ml 1-2 hours apart. Beware mineral oil enemas can cause perianal irritation and soreness. Out of precaution if you have a significant renal impairment the magnesium citrate can cause magnesium toxicity.
Having problems trying to pass hard or small pellet stools
Start with adding fiber to the diet and increase your fluid intake to increase the size and softness of the stools. If needed take a fiber supplement. I prefer Fibercon over Metamucil with the latter more likely to cause gas and bloating. When adding fiber either in the diet or supplement go slowly since rapid increase in fiber intake may cause cramping, bloating and excess gas until you are used to it. Stool softeners can also be used like Colace just be aware if you don’t really suffer from hard stools, softeners won’t help much.
Need a regular laxative
The best natural laxative is dried prunes. They have fiber and sorbitol. Try 6 dry prunes once or twice daily for which studies have shown works just as good as over-the-counter medications. If you don’t like prunes or they don’t help, start with Miralax which is over-the-counter and safe to use daily. It is usually well tolerated and can help keep you more regular. Like Miralax, milk of magnesium is another safe laxative to use regularly and is not absorbed by the intestines. It is my second choice. Start with a full dose at night then cutting back to ½ dose or even every two to three days when regular.
Need an occasional laxative
To main choices are Bisacodyl (Dulcolax) and Senna (Ex-lax). Both are known as irritative or stimulant laxatives that cause the muscles in the intestinal walls to contract to push stool through. Thus, the main side effect is cramping. They usually work within 6 hours or up to a day to produce a movement. They are reasonably safe to use 3-4 times a month but daily use can lead to tolerance and should be avoided.
Still having issues
Speak with a doctor. You may need some testing to find out the exact problem and maybe a prescription medication like Linzess, Motegrity or Amitiza may help if you have certain conditions. Also, some prescription medications can be ideal for the constipating side effects of narcotic pain killers like Relister or Movantik.